Real-World Treatment Patterns in Bipolar Disorder
The results of a large, real-world study by Jain et al suggest there may be an incongruence between current prescribing patterns and guideline recommendations for bipolar I disorder, with high use of antidepressants and benzodiazepines despite limited recommendations for these agents.

- Tina Matthews-Hayes, DNP, FNP-BC, PMHNP-BC
What do the results of this study mean for a practicing NP?
“These findings can help mental health providers understand the real-world treatment patterns for bipolar I disorder (BP-1) and provide a viewpoint into some of the treatment deviations from practice guideline recommendations. To help improve guideline-congruent care for patients with BP-1, antidepressant monotherapy for patients with suspected or confirmed BP-1 should be avoided, and guideline-endorsed treatments, such as mood stabilizers and atypical antipsychotics, should be prioritized. As nurses, we have existed in evidence-based practice since we were issued licenses as RNs. These findings remind me—and hopefully us—that we should make treatment decisions that are rooted in evidence rather than older practice trends.”
NP Psych Navigator contributors are paid consultants of AbbVie Inc.
Why was the research needed?
BP-1 can be a complex, chronic, and often severe mood disorder that may carry challenges in diagnosis and long-term management.1 Although there are various management options available for BP-1, including antipsychotics and mood stabilizers, there is limited real-world data on how these therapies are utilized in actual clinical practice.2
Patients with BP-1 may often seek treatment during a depressive episode, which studies have shown can lead to misdiagnosis as major depressive disorder (MDD).3,4 This can result in the administration of inappropriate treatment with antidepressant monotherapy. Antidepressant monotherapy in patients with BP-1 may increase the risk of mood instability, manic switching, or rapid cycling.2
Clinical practice guidelines are designed to help support evidence-based management, yet surveys show some clinicians remain unfamiliar with and nonadherent to these recommendations.1 To better understand how closely real-world practice aligns with guideline-based care, researchers conducted a large retrospective claims analysis of prescribing patterns among US patients newly diagnosed with BP-1. The primary objective was to examine real-world medication prescribing patterns across mood episodes and lines of therapy (LOTs) and to evaluate how closely these patterns aligned with established clinical practice guidelines.2
What did the researchers do?
This retrospective analysis used data from the IBM® MarketScan® Commercial Claims database between 2015 and 2018. Adult patients newly diagnosed with BP-1 were identified and included in the study if they had at least 12 months of continuous insurance coverage prior to diagnosis and 6 months after. Patients were excluded if they had evidence of schizoaffective disorder.2
Each patient’s treatment was characterized across episodes of illness, including depression, mania, mixed states, and remission, as well as across lines of therapy (LOTs) within each episode. A LOT was defined as a period of continuous treatment with one or more medications, with a change in medication initiating a new LOT.
The analysis characterized prescribing patterns both within each episode and across multiple episodes. The prescribed medications were categorized into classes, including atypical antipsychotics, mood stabilizers, antidepressants, benzodiazepines, stimulants, and other prescriptions.2
The treatment patterns were analyzed for their adherence to the treatment recommendations for BP outlined in the Florida Medicaid treatment guidelines.2
What were the key results of the study?
Of the 40,345 patients included in the study, the most common initial episode types were BP-1 depression (29.8%), BP-1 mania (12.8%), and BP-1 mixed features (12%). Approximately 90% of the participants received pharmacologic treatment as their first LOT (LOT1) during their first diagnosed mood episode, and approximately 80% went on to a second LOT. Across LOTs, antidepressants, benzodiazepines, and mood stabilizers were among the most common treatments prescribed for patients of all BP types. During LOT1, antidepressant monotherapy was prescribed for 12.9% of patients of all episode types, 14.5% of patients with BP-1 depression, and 12.4% of patients with BP-1 mania. However, guidelines recommend against the use of antidepressant monotherapy for BP-1 depression and mania (Table 1).2
In subsequent LOTs, the most common medication classes were antidepressants and benzodiazepines. The rate of antidepressant monotherapy use in these subsequent LOTs was approximately 10% for both patients with BP-1 depression and those with BP-1 mania. Moreover, although the current guidelines recommend atypical antipsychotics in managing BP, only about one-third of patients in the study were prescribed atypical antipsychotics.2
Additionally, the analysis indicated that only 11.8% of patients with BP-1 depression and 21.6% of those with BP-1 mania received the recommended first-line therapy (Figure 1).2 The likelihood of receiving a guideline-recommended treatment declined from LOT1 to LOT2, and this trend persisted for patients with BP-1 mania from LOT2 to LOT3, but not for patients with BP-1 depression (Figure 1).
| All | BP-1 Depression | BP-1 Mania | BP-1 Mixed | |
Total patients, N (%) | 36,587 (90.7%) | 11,005 (91.4%) | 4,503 | 4,424 |
| No. of regimens | 2,067 | 1,141 | 637 | 666 |
| Top 3 regimens | Mood stabilizer (9.6%) SSRIs (6.9%) Benzodiazepines (6.9%) | SSRI monotherapy (7.7%) Mood stabilizer (7.5%) Benzodiazepines (7.3%) | Benzodiazepines (8.8%) SSRIs (7.6%) Mood stabilizer (6.2%) | Mood stabilizer monotherapy (7.7%) Benzodiazepines (6.8%) SSRIs (6%) |
| % treated with AD monotherapy | 12.9% | 14.5% | 12.4% | 40.2% (mono or combination) |
Table 1. Treatment patterns during first episodes for all patients, patients with BP-1 depression, BP-1 mania, or BP-1 mixed episodes.2
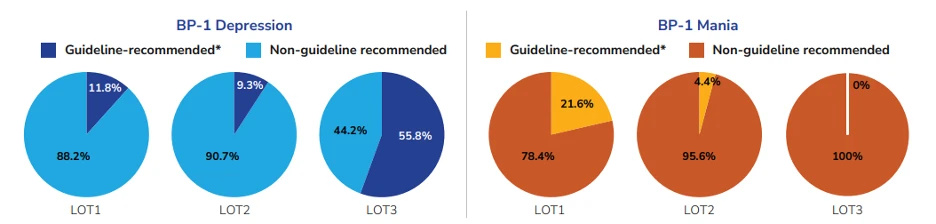
Figure 1. Percent of treated patients with BP-1 depression and BP-1 mania receiving therapy recommended by Florida Medicaid treatment guidelines* for LOTs 1-3.2
*Florida Medicaid Treatment Guidelines recommend atypical antipsychotics, mood stabilizers, or adjunctive therapy as initial treatments for BP-1 depression. For BP-1 mania, mood stabilizers and atypical antipsychotics as monotherapy or a combination of both for severe cases or those needing hospitalization, and electroconvulsive therapy for severe cases, are recommended.2
Limitations
- The study relied on claims data, which do not contain information on symptom severity, adherence, and reasons for medication changes.
- Data were limited to a commercially insured population, reducing generalizability.
- Medication use was based on filled prescriptions only; unfilled scripts and inpatient treatments were not included.
- Some medications have unapproved uses, and the diagnosis for which the medications were prescribed cannot be precisely determined for all cases.2
Why are these results important?
The study results suggest that there may be a gap between clinical guidelines and real-world management practices for BP-1, indicating that some BP-1 patients may not be receiving adequate or appropriate care.
The study found that antidepressants, especially as monotherapy, were frequently prescribed in BP-1 despite guidelines not recommending them as first-line therapy for BP-1 depression or mania. Antidepressant therapy is only recommended as a fourth-line agent adjunctive to mood stabilizers for BP-1 depression and is not recommended for BP-1 mania in the Florida Medicaid Drug Therapy Management Program.2 Antidepressant monotherapy can be associated with risks of mood destabilization and treatment-emergent affective switch in patients with bipolar mania.5,6 In addition, the findings revealed that guideline-recommended treatments such as atypical antipsychotics were underutilized.
The overall results highlight the disparity between real-world treatment patterns and recommendations from clinical practice guidelines, which may potentially impact patient outcomes for individuals with BP-1.
What’s next?
The study authors highlighted the need for greater consistency with guideline-recommended management strategies in treating patients with BP-1. They proposed that future research may be able to identify strategies to enhance adherence to guideline-recommended treatment regimens.2
References
- Gomes FA, Cerqueira RO, Lee Y, et al. What not to use in bipolar disorders: a systematic review of non-recommended treatments in clinical practice guidelines. J Affect Disord. 2022;298(pt A):565-576. doi:10.1016/j.jad.2021.11.007
- Jain R, Kong AM, Gillard P, Harrington A. Treatment patterns among patients with bipolar disorder in the United States: a retrospective claims database analysis. Adv Ther. 2022;39(6):2578-2595. doi:10.1007/s12325-022-02112-6
- McIntyre RS, Calabrese JR. Bipolar depression: the clinical characteristics and unmet needs of a complex disorder. Curr Med Res Opin. 2019;35(11):1993-2005. doi:10.1080/03007995.2019.1636017
- Vossos H, Nwosu-Izevbekhai O. Mood disorders and rapid screening: a brief review. J Ment Health Clin Psychol. 2024;8(2):51-54. doi:10.29245/2578-2959/2024/2.1314
- Viktorin A, Lichtenstein P, Thase ME, et al. The risk of switch to mania in patients with bipolar disorder during treatment with an antidepressant alone and in combination with a mood stabilizer. Am J Psychiatry. 2014;171(10):1067-1073. doi:10.1176/appi.ajp.2014.13111501
- Salvadore G, Quiroz JA, Machado-Vieira R, et al. The neurobiology of the switch process in bipolar disorder: a review. J Clin Psychiatry. 2010;71(11):1488-1501. doi:10.4088/JCP.09r05259gre
This summary was prepared independently of the study’s authors.
This resource is intended for educational purposes only and is intended for US healthcare professionals. Healthcare professionals should use independent medical judgment. All decisions regarding patient care must be handled by a healthcare professional and be made based on the unique needs of each patient.
ABBV-US-02192-MC, Version 1.0
Approved 09/2025
AbbVie Medical Affairs
