Patient Case Navigator: Differentiating Bipolar I Disorder From Major Depressive Disorder
Welcome to the Patient Case Navigator, an interactive learning experience for Nurse Practitioners. Please use the Next or Previous buttons at the bottom of the page to move forward or backwards.
Introduction
Learning Objectives
Learning Objectives
- Differentiating the characteristics between major depressive disorder (MDD) and bipolar I disorder (BP-1) and challenges identifying these features
- Probing questions to ask a patient with MDD who develops new symptoms
- A patient-reported screening tool to help assess patients for BP-1
- Potential management options for this patient after arriving at a new diagnosis
Watch the video:
Patient Chart Review
History of Present Illness
Medical History
Jenna's Timeline
History of Present Illness
Jenna is a 29-year-old woman who was previously diagnosed with major depressive disorder (MDD). Twelve weeks ago, she presented to her primary care physician, Dr Jones, with a chief complaint of depressed mood, diminished interest in her usual hobbies and activities, excessive sleeping, increased appetite, and weight gain. At that time, Jenna scored 19 on her Patient Health Questionnaire-9 (PHQ-9), which is suggestive of moderately severe depression, so she was diagnosed with undergoing a current major depressive episode (MDE). Jenna began pharmacotherapy with a serotonin and norepinephrine reuptake inhibitor (SNRI). After 4 weeks of initial SNRI therapy, Jenna reported mild improvements in her mood at a follow-up visit (PHQ-9 score of 16), where a dose adjustment was made. Her second follow-up at week 8 resulted in a PHQ-9 score of 14 and another SNRI dose increase. Around week 10, however, she developed sleep troubles and some irritability.
Medical History
Jenna has intermittent asthma for which she uses an inhaler. She is adherent to her combined oral contraceptive pills for birth control and the SNRI that she started 12 weeks ago. She has had 2 trials of selective serotonin reuptake inhibitors (SSRI) for MDD previously.
Jenna drinks 1 to 2 cups of coffee in the morning daily. She has 1 to 2 alcoholic beverages weekly with her partner. Jenna denies a history of smoking or other drug use.
Timeline of Jenna's Present Illness
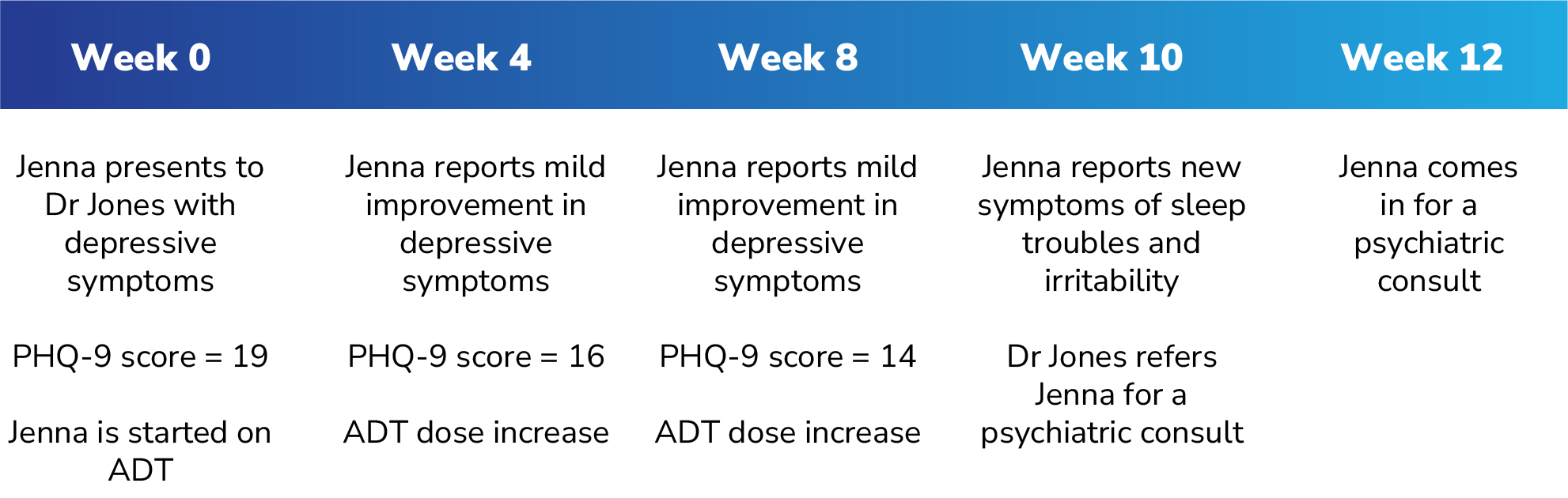
PHQ-9 = Patient Health Questionnaire-9, ADT = antidepressant therapy
Watch the video:
Patient Interview
Current Symptoms
History of Episodes
Evaluating Jenna's Current Symptoms 1-3 :
- Changes in sleep
- Changes in appetite
- Depressive symptoms
- Psychomotor retardation
- Agitation/irritability/racing thoughts
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Publishing; 2013. 2. Bobo WV. Mayo Clin Proc. 2017;92(10):1532-1551. 3. Yatham LN, et al. Bipolar Disord. 2018;20:97-127.
Episode Evaluation
- # of lifetime manic/depressive episodes
- Index episode
- Last episode
- Triggers/precipitants
- Age of onset
1. The Psychiatric Interview. Psych DB. 2024. 2. Mitchell PB, et al. Bipolar Disord . 2008;10(1Pt2):144-152.
Watch the video:
Quiz #1
Current Medical History
Quiz #2
Introducing the Rapid Mood Screener
Screening for BP-1
Rapid Mood Screener
New Diagnosis
BP-1 Symptoms Prevalence
Screening for BP-1
During the patient interview, given his suspicions on a diagnosis other than MDD, Tony has Jenna fill out the Rapid Mood Screener (RMS), a self-administered screening tool designed to help differentiate BP-1 from MDD in patients with depressive symptoms.1
1. McIntyre RS, et al. Curr Med Res Opin. 2021;37(1):135-144.
Rapid Mood Screener
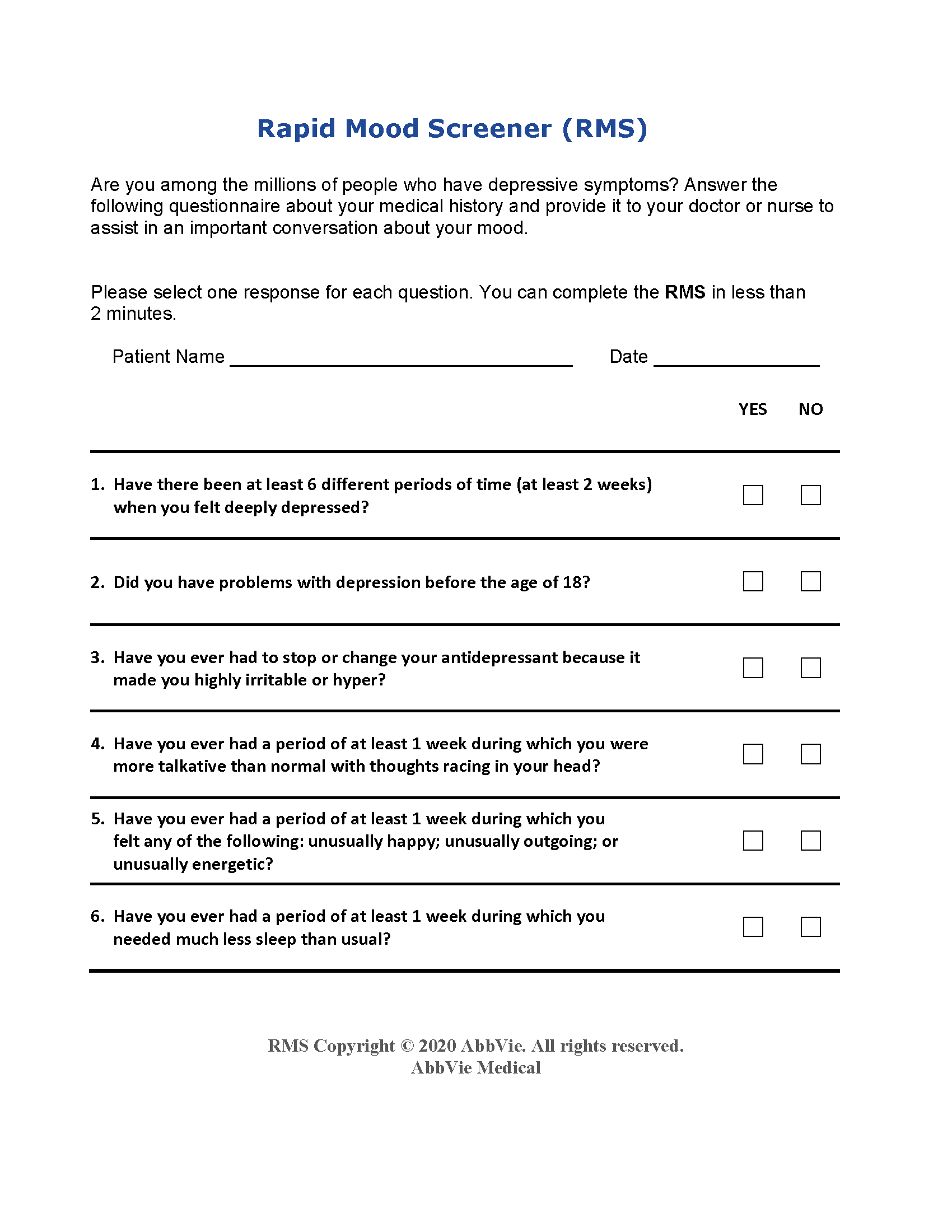
The RMS is not a diagnostic tool. The RMS tool was developed with funding and input provided by AbbVie and external experts, who received financial support from AbbVie for research, honoraria and/or consulting services depending on the author. 1. McIntyre RS, et al. Curr Med Res Opin. 2021;37(1):135-144.
New Diagnosis
Based on Jenna's and her partner's combined report, as well as her physical examination and medical history, Tony considers the shift in mood and new symptoms as potentially indicative of a different diagnosis. Jenna's response to her SNRI regimens is particularly suggestive, as patients with BP-1 who are started on an antidepressant may undergo a treatment-emergent affective switch (TEAS).
TEAS: A switch in mood polarity from depression to mania or hypomania that can be induced by certain medications, including antidepressant monotherapy1,2
1. Moller HJ, et al. Expert Rev Neurother. 2004;4(6 Suppl 2):S3-S8. 2. Salvadore G, et al. J Clin Psychiatry. 2010;71(11):1488-1501.
BP-1 Symptoms Prevalence
- Symptoms of depression in BP-1 closely resemble those in MDD.1
- Depressive symptoms are the most commonly reported symptom in patients with BP-1.2
- Patients with BP-1 may experience multiple depressive episodes in their lifetime.3
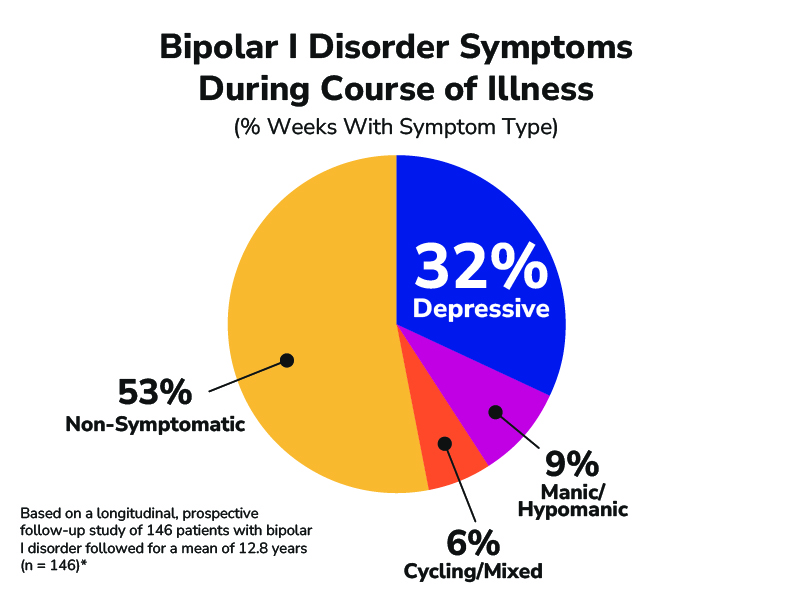
*National Institute of Mental Health Collaborative Depression Study (1978 to 1981): weekly symptom severity level based on the 6-point LIFE Psychiatric Status Rating (PSR) scale for depression and mania plus the 3-point PSR scale for rating minor depression/dysthymia, hypomania, DSM-4 atypical depression, DSM-3 adjustment disorder with depressed mood, and Research Diagnostic Criteria cyclothymic personality. 1. Culpepper L. Prim Care Companion CNS Disord. 2014;16(3):PCC.13r01609. 2. Judd LL, et al. Arch Gen Psychiatry. 2002;59:530-537. 3. Yatham LN, et al. Bipolar Disord. 2018;1-74.
Watch the video:
Quiz #3
Jenna's Management Plan
Management Plan
Management Plan
Tony arrives at a diagnosis of bipolar I disorder and establishes a new management plan. He suggests starting Jenna on an atypical antipsychotic. Jenna objects at first, becoming agitated and stating that she is not psychotic. Tony dispels the stigma by explaining the history of the medication class. He elaborates on the rationale behind his thinking and discusses the safety and tolerability aspects of the medication class. He additionally suggests starting cognitive behavioral therapy (CBT). He schedules a follow-up in 2 weeks to check how the new medication is working for her.1
1. American Psychiatric Association. Practice Guidelines for the Treatment of Patients with Bipolar Disorder. 2nd ed. American Psychiatric Association; 2002.
Watch the video:
Quiz #4
Conclusion
Summary Points
Predictive Factors
Manic Symptoms
RMS
Treatment Options
Summary Points
- A study showed that patients with bipolar I disorder may spend 32% of the time in a depressed state compared to 9% of the time in a manic state over the course of their illness. Also, BP-1 patients usually present to a primary care physician when experiencing depressive symptoms.1
- Patients can experience a delay of up to 5 to 10 years between symptom onset and receiving a correct diagnosis of BP-1.2
- Treatment-emergent affective switch (TEAS) is a switch in mood polarity from depression to mania or hypomania that is induced by certain medications, including antidepressant monotherapy.3,4
1. Judd LL, et al. Arch Gen Psychiatry. 2002;59(6):530-537. 2. Phillips ML, et al. Lancet. 2013;381(9878):1663-1671. 3. Moller HJ, et al. Expert Rev Neurother. 2004;4(6 Suppl 2):S3-S8. 4. Salvadore G, et al. J Clin Psychiatry. 2010;71(11):1488-1501.
Differential Features of MDD and BP-1
Major Depressive Disorder
- Negative family history of bipolar disorder
- Initial insomnia/reduced sleep
- Appetite and/or weight loss
- Normal or increased activity levels
- Somatic complaints
- Later onset of first episode (> 25 years)
- Fewer prior episodes (< 5 episodes)
- Longer duration of episode (> 6 months)
Bipolar Disorder
- Positive family history of bipolar disorder
- Hypersomnia/increased daytime napping
- Increased appetite/weight gain
- Atypical depressive symptoms
- Psychomotor retardation
- Manic symptoms present (eg, agitation/irritability/racing thoughts)
- Earlier onset of first episode (< 25 years)
- Multiple prior episodes (≥ 5 episodes)
This is not a diagnostic tool and is not intended to replace a clinical evaluation by a healthcare provider. 1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Publishing; 2013. 2. Bobo WV. Mayo Clin Proc. 2017;92(10):1532-1551. 3. Yatham LN, et al. Bipolar Disord. 2018;20:97-127.
APA Diagnostic Criteria for Mania
A distinct period of abnormally and persistently elevated, expansive, or irritable mood and abnormally and persistently increased goal-directed activity or energy, lasting at least 1 week and present most of the day, nearly every day (or any duration if hospitalization is necessary).
During the period of mood disturbance and increased energy or activity, 3 (or more) of the following symptoms (4 if the mood is only irritable) are present to a significant degree and represent a noticeable change from usual behavior1:
- Inflated self-esteem or grandiosity
- Decreased need for sleep
- Racing thoughts
- Distractibility
- Increase in goal-directed activity (this may be socially, at work or school, or sexually) or psychomotor agitation or restlessness
- Excessive involvement in activities that have a high potential for painful consequences
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Publishing; 2013.
RMS
- The Rapid Mood Screener (RMS) is a pragmatic, self-administered screening tool designed to differentiate BP-1 from MDD in patients who have already been diagnosed with MDD.
- It contains 6 "Yes" or "No" questions that evaluate 3 symptoms of depression and 3 symptoms of mania.
- A patient answering "Yes" to 4 or more items signals a very high likelihood of having BP-1.
- When compared to the Mood Disorder Questionnaire (MDQ), the RMS demonstrated a sensitivity of 88% and a specificity of 80%, while those of the MDQ were 86% and 78%, respectively.
- A positive screen on the RMS would subsequently require a more comprehensive evaluation by a mental healthcare provider to confirm a BP-1 diagnosis.1
The Rapid Mood Screener (RMS) is not a diagnostic tool. The RMS tool was developed with funding and input provided by AbbVie and external experts, who received financial support from AbbVie for research, honoraria and/or consulting services depending on the author. 1. McIntyre RS, et al. Curr Med Res Opin. 2021;37(1):135-144.
Treatment Options
APA Management Options for Bipolar I Disorder
-
Pharmacotherapy
- Mood stabilizers
- Antipsychotic medications
- Monotherapy with antidepressants is not recommended.
- Psychotherapy, in addition to pharmacotherapy, has also been shown to help improve patient outcomes.1
1. American Psychiatric Association. Practice Guideline for the Treatment of Patients with Bipolar Disorder. 2nd ed. American Psychiatric Association; 2002.
Watch the video:
Alan "Tony" Amberg is a paid consultant for AbbVie Medical Affairs and was compensated for his time.
Recommended on NP Psych Navigator

Clinical Article
Treatment Patterns, Healthcare Resource Utilization, and Costs Associated With the Use of Atypical Antipsychotics as First vs Subsequent Adjunctive Treatment in Major Depressive Disorder
This retrospective study by Jain et al aimed to assess the use of atypical antipsychotics as first add-on treatment vs later add-on treatment in patients with MDD and to evaluate the potential impact of atypical antipsychotic line of therapy (LOT) on healthcare resource utilization (HCRU).



